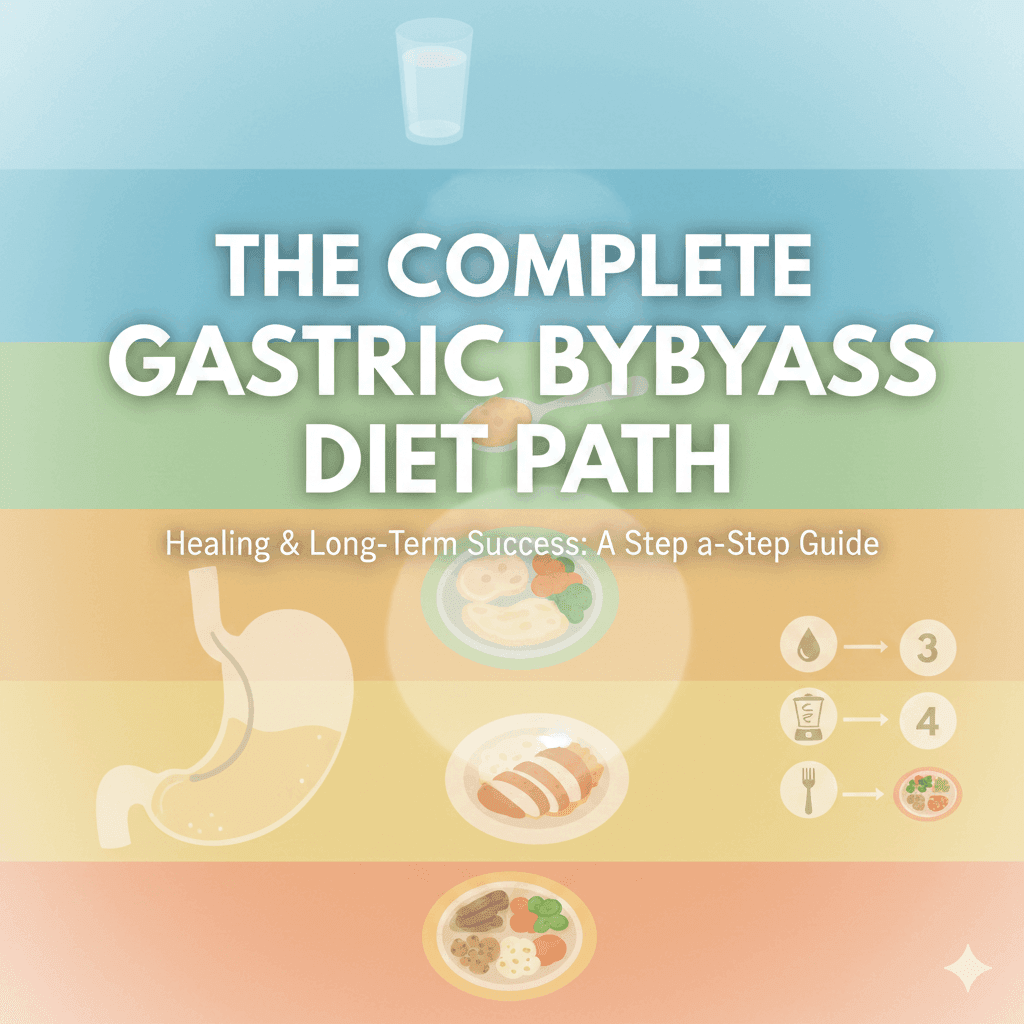
If you’re reading this, chances are you’ve recently had gastric bypass surgery—or you’re preparing for life after it. I want to begin by validating that decision. Choosing gastric bypass is not “the easy way out.” It is a medically complex, life-altering intervention that requires courage, commitment, and a willingness to change long-standing habits.
The post-operative diet is not simply about weight loss. In fact, weight loss is a byproduct. The real goal is healing and protecting your new anatomy—specifically your gastric pouch, the anastomosis (the surgical connection between your pouch and small intestine), and the altered digestive flow that now bypasses the pyloric valve.
Your stomach capacity is now dramatically reduced—often to 15–30 mL initially. That means eating is no longer intuitive; it must be intentional. This guide walks you through each dietary phase with clinical precision and deep empathy, explaining not just what to do, but why these guidelines exist. When you understand the reasoning, compliance becomes far easier—and long-term success becomes realistic.
Phase 1: Clear Liquids (Days 1–7)
The Primary Goal: Hydration Without Stressing the Anastomosis
What’s Allowed
During the first week, your digestive system is in a critical healing window. The anastomosis is fragile, swollen, and vulnerable to pressure.
Approved clear liquids typically include:
- Water
- Sugar-free electrolyte drinks
- Clear broth (fat-free)
- Sugar-free gelatin
- Decaffeinated herbal tea
No calories are required at this stage. Nutrition is secondary to hydration and tissue protection.
Why “Sipping, Not Gulping” Is Non-Negotiable
Your new gastric pouch has no stretch capacity early on. Gulping creates rapid pressure, which can:
- Cause nausea or chest discomfort
- Stress the anastomosis
- Increase risk of leaks or vomiting
Clinical guideline:
Take small sips every 5–10 minutes, aiming for 48–64 oz per day by the end of week one.
Preventing Dehydration (The #1 Cause of Early Readmission)
Dehydration happens quickly post-op because:
- Thirst signals are blunted
- Swelling limits intake
- Nausea discourages drinking
Signs of dehydration include dark urine, dizziness, fatigue, and headaches. If you cannot keep liquids down consistently, this is not something to “push through.” Early intervention prevents IV fluids and setbacks.
Phase 2: Full Liquids & Pureed Foods (Weeks 2–3)
The Goal: Introduce Protein Without Mechanical Stress
This phase marks your first nutritional intake, but the digestive rules remain strict.
Texture Is Everything: The “Cottage Cheese Consistency” Rule
All foods must be:
- Smooth
- Lump-free
- Pourable from a spoon
Why? Because solid particles can lodge near the anastomosis, causing pain, vomiting, or obstruction.
Acceptable foods include:
- Protein shakes (low sugar, high protein)
- Blended low-fat soups
- Plain Greek yogurt (no fruit chunks)
- Pureed eggs or beans
Protein Supplements: Why They’re Essential Now
At this stage, protein is medicine. Your body is healing surgical wounds, preserving lean mass, and adapting hormonally.
Clinical target:
- 60–80 g protein/day, primarily from liquids
Without adequate protein, patients experience:
- Muscle loss
- Hair thinning
- Poor wound healing
- Fatigue
Protein shakes are not optional—they are temporary clinical tools.
Phase 3: Soft Foods (Weeks 4–8)
The Goal: Teach the Pouch How to Handle Texture
Now we begin retraining your digestive system—slowly.
Lean Protein Comes First (Always)
Your pouch capacity is still limited (often ½ cup or less). If you fill it with carbohydrates, protein gets displaced.
Best tolerated options:
- Soft scrambled eggs
- Flaked fish
- Moist, shredded chicken
- Ground turkey
Eat protein first, then soft vegetables if space allows.
Why Skinless and Seedless Matters
Skins, seeds, and fibrous strands are difficult to break down mechanically—remember, you no longer have the pyloric valve regulating food emptying.
These can:
- Cause blockage
- Trigger nausea
- Sit heavily in the pouch
Vegetables must be:
- Well-cooked
- Peeled
- Mashed with a fork
Phase 4: Stabilization – The “New Normal”
The Goal: Lifelong Eating With Awareness
This phase is not an endpoint—it’s a transition into permanent bariatric eating.
Reintroducing Solid Foods Safely
New foods should be tested one at a time. Tolerance varies widely. A food that causes discomfort today may be tolerated months later.
Permanent rules include:
- Small bites
- Thorough chewing (20–30 chews per bite)
- Meals lasting 20–30 minutes
Fullness now feels different—pressure, tightness, or a runny nose—not hunger relief.
The Non-Negotiables of Gastric Bypass Nutrition
The 30-Minute Rule (No Drinking With Meals)
Drinking with meals:
- Flushes food through the pouch too quickly
- Reduces satiety
- Increases dumping risk
Rule:
- Stop drinking 30 minutes before meals
- Resume 30 minutes after
This protects pouch capacity and nutrient absorption.
Protein-First Prioritization
Protein:
- Preserves muscle
- Stabilizes blood sugar
- Supports long-term weight maintenance
Every meal starts with protein. Always.
Vitamin & Mineral Supplementation (Lifelong)
Because gastric bypass bypasses absorption sites, supplementation is mandatory.
Core supplements include:
- Vitamin B12 (sublingual or injection)
- Iron (especially for menstruating patients)
- Calcium citrate (not carbonate)
- Vitamin D
Deficiencies can lead to anemia, neuropathy, bone loss, and fatigue—even years later.
Dumping Syndrome: What It Is and How It Feels
Dumping syndrome occurs when sugar or high-fat foods rapidly enter the small intestine.
Symptoms include:
- Nausea
- Diarrhea
- Sweating
- Heart palpitations
- Dizziness
It is not dangerous—but it is deeply unpleasant. Avoidance comes from:
- Limiting sugar
- Eating slowly
- Separating liquids from solids
The Psychological Shift: Head Hunger vs. Belly Hunger
After surgery, hunger hormones change—but emotional habits don’t disappear.
Head Hunger
Driven by:
- Stress
- Routine
- Social cues
- Emotions
Belly Hunger
Physical signs include:
- Low energy
- Stomach sensations
- Gradual onset
Learning to pause and identify the source of hunger is one of the most important post-op skills. Many patients grieve food. That grief is real—and support is appropriate, not a failure.
Daily Protein Tracker (Example)
| Time | Food Source | Protein (g) |
|---|---|---|
| Breakfast | Protein shake | 25 |
| Lunch | Soft scrambled eggs | 18 |
| Snack | Greek yogurt | 12 |
| Dinner | Shredded chicken | 20 |
| Total | 75 g |
Tracking isn’t about control—it’s about adequacy.
Long-Term Success Is Built on Respect for Your Anatomy
Gastric bypass changes your digestive system permanently—but success depends on how well you honor that change. When patients struggle years later, it is rarely due to “lack of willpower.” It is almost always a breakdown in structure, understanding, or support.
This diet path is not punishment. It is protection—of your pouch, your anastomosis, your nutrient status, and your future health.
If there’s one message I want you to carry forward, it’s this:
You are not failing if you need guidance. You are succeeding by seeking it.
Healing is not linear. But with knowledge, patience, and consistency, long-term success is absolutely achievable.